Hot Flushes
Understanding Hot Flashes: Symptoms, Causes, and Solutions
Hot flashes are the bane of many a peri- or post-menopausal woman’s existence – especially since they are linked to insomnia and depression. Because they have such a negative impact on quality of life, they are one of the most common reasons women make doctor appointments while in their forties and fifties. The typical age range for developing moderate-to-severe hot flashes is between the ages of 45 and 49. They tend to last for an average of ten years.
While the mechanisms behind this irritating symptom aren’t fully understood, diet and lifestyle changes may help. I hope to give you some things to consider and some tips for lessening both the frequency and severity of hot flashes.
What do Hot Flushes Feel Like?
Hot flushes/flashes tend to come on suddenly (hence, “flash”) and involve a number of distressing and uncomfortable symptoms:
- Sudden warmth of face, neck, and chest
- Sweating
- Increased pulse rate
- Chest tightness
- Anxiety
- Flushed skin, sometimes blotchy
- Sometimes followed by a chill
If it’s not enough to have these unpleasant mini sauna sessions during the day, they are often accompanied by night sweats that wake you from a pleasant slumber. This can lead to insomnia, sleep deprivation, and feelings of hopelessness and depression.
Triggers
If you’re not sure what triggers you, consider keeping a small notebook with you or notes on your phone. Then make note of when hot flushes come on and what happened right before. The 5 most commonly reported triggers of hot flashes are the following:
- Stress/Emotional situations (59%)
- External heat (44%)
- Confining space (38%)
- Alcohol (20%)
- Caffeine (17%)
Note that these triggers simply bring on a hot flush. They aren’t actual causes of the imbalance.
When we look deeper into what the underlying causes of hot flushes are – there are at least seven, most of which you can control.
7 Causes of Hot Flashes
The mechanism isn’t completely understood, but medical experts believe hot flushes originate in the brain and are caused by the dysregulation of the temperature control mechanism in the hypothalamus. Certain hormones/catecholamines, adrenaline (epinephrine), noradrenaline (norepinephrine), as well as thyroid hormones are likely involved.
While there is a genetic component, the actual causes behind dysregulation in the hypothalamus are related to some type of imbalance or deficiency:
1. Blood Sugar Imbalance
Essentially, what this means is that anything that puts stress on the brain and body can be a contributor to hot flushes. That includes blood sugar issues and hypoglycemia. Studies have found that a drop in blood sugar can trigger hot flushes. Women were more likely to have hot flushes if they went a longer time between meals.
This is one reason why I encourage my menopausal ladies to have a PFF based breakfast (Protein / Fat / Fibre).
2. Low or Dropping Estrogen Levels
It is no surprise that hot flushes are most common in women entering peri- or menopause because that’s when estrogen production starts dropping.
How do you know if you have low estrogen? Symptoms of low estrogen include:
- Hot flashes
- Weak bones
- Osteopenia and osteoporosis
- Poor sleep
- Sagging and/or dry skin
- Hair thinning or loss
- Weaker cognitive functions, such as forgetfulness
- Vaginal thinning and dryness
- Incontinence
- Loss of sex drive
- Irregular periods or no periods
What researchers are learning about estrogen is that it’s important to have a balance of estrogen-promoting and estrogen-limiting activities for us to have healthy hormone levels. Both estrogen dominance and low estrogen can be a problem, and that’s where taking phytoestrogens from plants like flax and hops can help. Phytoestrogens can serve as weak estrogens that can help support low estrogen levels, yet replace more potent estrogens so that we don’t become estrogen dominant.
While scientists don’t know exactly why low estrogen levels can cause hot flashes, I believe that blood sugar imbalance and inflammation, when combined with dropping estrogen levels, is the perfect storm.
The good news is that there are food and supplements that can raise estrogen levels – I’ve written an article with oestrogen raising tips here.
3. Low Progesterone
Progesterone is also likely involved in hot flushes. Estrogen can cause anxiety when out of balance with progesterone, as progesterone has an anti-anxiety effect on the body. As progesterone levels decline and fail to balance estrogen, the body is also put in more of a stressed, high adrenaline state. Again, stress is the top trigger associated with hot flushes.
4. Inflammation
Additionally, low-grade systemic inflammation has been tied to hot flashes. What can cause chronic systemic inflammation? Certainly, dietary choices – an inflammatory diet or eating foods that cause inflammation in an individual (like food allergies or intolerances) can lead to chronic inflammation.
A study of postmenopausal women and diet found that those who consumed a higher antioxidant diet had fewer hot flashes.
Many women in my clinic, my community and on my program have reported a reduction of hot flashes with a change of diet – especially after removing inflammatory foods, such as gluten and dairy, and reducing their intake of sugar and coffee (or completely cutting out all caffeine).
5. Mineral Deficiencies
Mineral deficiencies, such as magnesium, and possibly zinc and selenium may also contribute to hot flashes.
6. Ethnicity
A study of over 16,000 American women found that African Americans and Hispanics were more likely to experience hot flashes than other ethnic groups, including Caucasians.
7. Lifestyle factors: Smoking
Smoking is one of the few lifestyle factors that is consistently associated with hot flashes. Women who smoke are more likely to experience hot flashes than nonsmokers. In fact, over the course of 6 years, smokers had a 60% increased risk of vasomotor symptoms like hot flashes as compared to nonsmokers.
Solutions for Hot Flashes
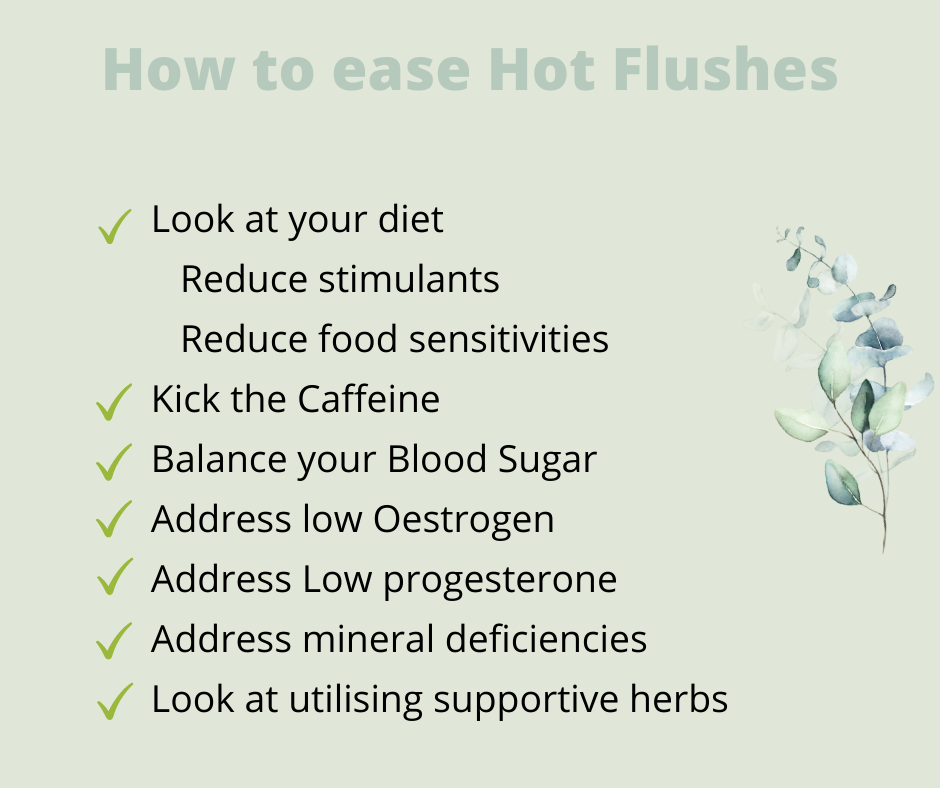
Diet
Diet is really important here. Hot flushes are yet another sign of hormone imbalance, and my first line therapy for balancing hormones has always been food.
Here are some things to consider:
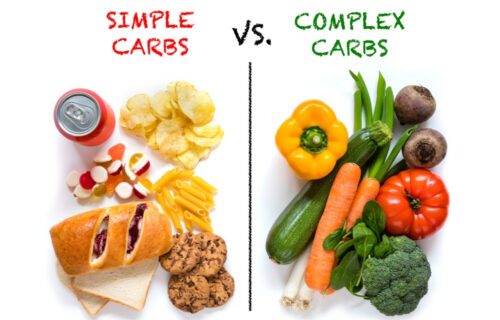
- Is your diet generally inflammatory or anti-inflammatory?
- Are you intolerant to some of the otherwise healthy foods you’re eating? Gluten and dairy are common culprits.
- Is your diet causing blood sugar dysregulation?
- Do you consume stimulants? Sugar, alcohol, caffeine…?
- If you answered “yes” to any of the above, you may want to consider trying changing some of this.
Kick the Caffeine
When addressing hot flashes through diet, I hate to break it to you, but it’s really best to also remove coffee. Unfortunately, coffee contributes to estrogen dominance, and, according to this study, caffeine may increase blood sugar levels.
In my experience, many women who have given up coffee and caffeine report better sleep within days, fewer hot flashes, and other benefits over time.
Balance Blood Sugar
Unbalanced blood sugar levels can cause the body to stay stuck in an inflammatory state, leading to the overproduction of stress hormones and then a general state of hormone imbalance, including estrogen dominance. We know from studies that blood sugar problems and inflammation can contribute to hot flushes.
To balance your blood sugar, I recommend starting your day with a PFF breakfast.
Reduce Inflammation
When you implement all of the above suggestions, your inflammation levels are bound to come down. If you feel like you need additional help in lowering inflammation, try supplements containing Boswellia (frankincense) and turmeric as the hero ingredients.
Address Low Progesterone
Low progesterone may also lead to hot flushes. Progesterone is a hormone that helps balance the effects of estrogen in the body. It’s very sensitive to stress in our lives. There are a few nutrients that can help boost your progesterone naturally; however, for many women, topical progesterone is a more efficient way to raise your progesterone to healthy levels. This study found that a form of progesterone reduced hot flashes by up to 80%.
Increase Low Estrogen
Low estrogen is another hormonal contributor to hot flushes. Phytoestrogens, estrogens naturally occurring in plants, may be the best natural solution. A review of 62 studies using plant-based therapies for menopause symptoms in 6653 women found that phytoestrogens, such as lignans found in flax, helped reduce hot flashes.
There are three types of phytoestrogens:
- Lignans (including enterolactone and enterodiol)
- Isoflavones (genistein, daidzein, and biochanin A)
- Coumestans
The highest concentration of phytoestrogens is found in lignans.
Herbal Recipes for Hot Flushes
Certain herbs have been shown to be helpful for cooling those hot flashes:
- Dong Quai .
- Chaste berry (otherwise known as Vitex)
- Black cohosh
- Red clover
- Maca
Address Mineral Deficiencies
Mineral deficiencies may also contribute to hot flushes. Try adding magnesium in the form of magnesium glycinate.
In Summary
Remember: Take away before you add. Remove the high carb, inflammatory, glucose-spiking foods. Remove foods you are sensitive to. Lower your stress and inflammation. Add in colourful whole foods, and, start to include some of the tips listed above.